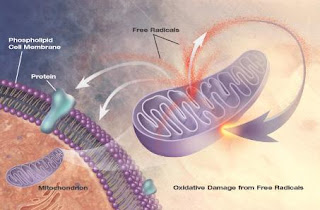
In clinical circles, the term "oxidative stress" is used frequently. You may have heard people talk about oxidative stress-inducing "free radicals" and how their influence is counteracted by "antioxidants." Simply put, oxidative stress refers to a chemical instability that disrupts the function of cell membranes, enzymes and overall cellular function. Oxidative processes are a normal part of human physiology but our built-in checks and balances system allows "antioxidants" to blunt any potential harm. Many of these antioxidants are derived from our diet while other are synthesized by our body.
One study found that higher levels of oxidative stress were associated with further decline in function among MS patients. Interestingly, this decline happened even though the appearance of lesions on MRI did not change.The authors conclude, "This process [oxidative stress] could be at least partially responsible for ongoing functional decline in SPMS (secondary progressive multiple sclerosis)." Mult Scler 2010 Oct 4 (epub)
In a sense, it is probably best to regard oxidative stress as a byproduct of the disease process rather than as a direct cause. Let's think of it this way; if a team of bandits came through your neighborhood setting houses on fire, there is going to be a massive amount of destruction. As the fires blaze away, the bandits enjoy the cover of smoke and chaos and set even more houses on fire. That team of bandits can be compared to any disease process; in our case, MS.
Oxidative stress is likened to the flames coming out of the homes. While the bandits were the cause of the problem, the flames themselves lead to destruction, fear and bodily harm as well. It is in our interest to put out those flames.
A paper out of the University of Wisconsin-Madison compares the threat of the bandits versus the threat of the fires. The authors describe the attack on myelin by immune cells and go on to state, "Secondary to these events, however equally destructive, is the generation of inflammatory-mediated reactive oxygen and nitrogen species generated by persistently activated microglia and astrocytes." They suggest that by increasing our production of antioxidants (and detoxification agents), we may "attenuate pathogenesis of autoimmune diseases such as MS..." Toxicol Sci 2010 Apr;114(2):237-46.
Regarding the primary treatment of MS with interferon and other pharmaceuticals, one author writes,
"disease progression, although typically delayed with these agents, remains inevitable in most patients and constitutes a significant limitation of the currently available treatments....a better understanding of pathophysiologic factors in MS--such as the role of neurotrophic growth factors and oxidative stress--are changing the ways that efficacy is measured and how new agents are developed." Am J Managed Care 2010 Sep; 16(8 Suppl):S211-8.
Clearly, oxidative stress is a force to be reckoned with. In the next post, I'll discuss strategies to counter oxidative stress.